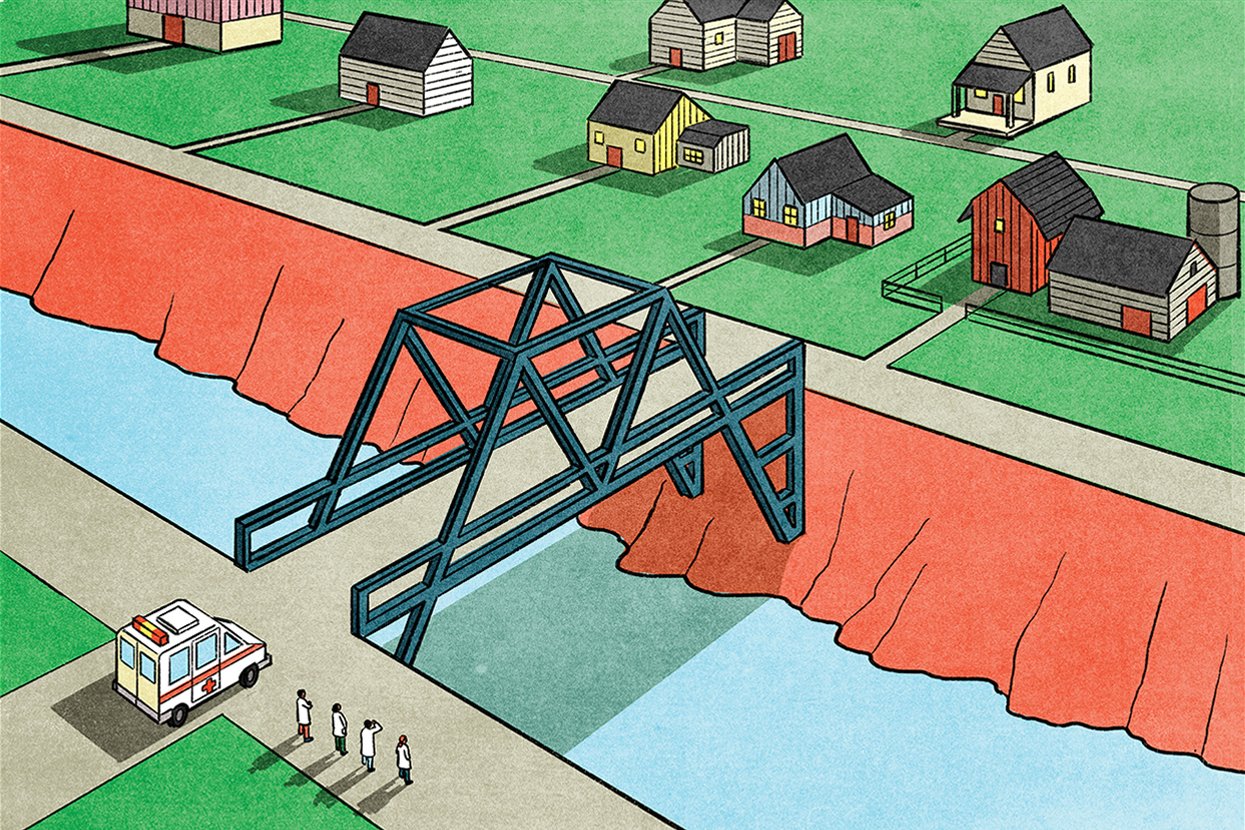
Bridging the Gap
Five physician assistant students share the ways they are working to help reduce health disparities among population groups.
By Rich Polikof
Illustration by Klaus Kremmerz
Urban, underserved, and rural populations are at higher risk for mental health disorders and substance abuse disorder, and they report higher numbers of health concerns such as heart disease and diabetes. A recent grant from the Health Resources and Services Administration aimed at increasing primary care training, with an emphasis on rural and underserved areas, has allowed the U to create the HRSA Primary Care Scholar program. Students receive a $16,000 scholarship and a clinic-based research project at one of HRSA’s primary care training sites. Five Spencer Fox Eccles School of Medicine students tell us about those projects.
JESSICA BARNEY
The Project: I did a retrospective data analysis to determine the effects of the COVID-19 pandemic on management of diabetes. I completed the project in partnership with Emery Medical Center, which is in my hometown of Castle Dale, Utah.
Building Community Through Relationships: I grew up in a small town where family, teachers, friends, and neighbors always supported me in achieving my goals. This instilled in me the desire to help build up communities while helping individuals and building relationships with them.
PETER CASTILLO
The Project: I compared medication adherence rates between patients who receive their prescription medications via a consolidated mail outpatient pharmacy versus a traditional in-person medication pickup. The project occurred in the Fort Duchesne Indian Health Service (IHS) Unit on the Uintah and Ouray Indian Reservation. The most memorable part of the project was learning how to navigate the unique IHS health care system at the ground level. Talking to and learning about the culture of the varying tribes who receive care at the clinic was a humbling experience and put into perspective how much more there is to know about other underserved communities in our country.
Offering a Familiar Perspective: I was born and raised in an underserved rural community. I’ve experienced firsthand the lack of resources and opportunities many underserved areas face. My community raised me, and I would not be in this position without them. Being a minority in a predominantly minority community, a homegrown product, and coming from a disadvantaged background, I offer my community advocacy and a familiar perspective.
PEI CHEN
The Project: I looked at ways of improving health outcomes for historically marginalized communities by increasing HbA1c testing rates of diabetic patients from those communities, which is the first step in achieving better blood glucose control and avoiding some of the long-term complications of diabetes.
Becoming a Strong Generalist: I’m a scholar in the Urban Underserved track. Prior to PA school, I did field-based work and acted as the extension of the primary care clinic into the home for patients living in SROs and shelters. I saw the number of medical challenges, both acute and chronic, that these patients faced. It was clear that good access to specialty care was needed, but what spoke to me even more strongly was the need for a strong generalist and advocate who would know both the patient and the health care system—and stay with them long-term to create behavior change.
COLTON KESLER
The Project: I worked closely with the quality assurance director of the Indian Health Services clinic on the Uintah and Ouray Indian Reservation. I did a retrospective chart review and analysis regarding medication adherence and visits to the pharmacy/clinic. I learned how seriously the staff and clinicians at IHS take the health of the community, and I was amazed at their dedication to the residents of the reservation. I was honored to do some groundwork to help them with their analysis and interventions.
Increasing the Availability of Care: It’s easy to be passionate about rural health care when you come from a rural area. I know how challenging it can be to get the care you need. Growing up in Central Utah presented interesting challenges whenever someone was sick or injured—even more so when resources in the small local hospital/clinic didn’t have what we needed. Increasing availability of care in those rural areas is so important.
WALIAH WYATT
The Project: I collaborated with four other PA students with the Utah Department of Health. We sought to measure the success of their Living Well with Chronic Pain Program, in addition to making recommendations for program improvement based on patient survey data.
Giving Back: I was raised in a rural area of New York and saw firsthand the limitations of primary care for underserved areas. I am the fourth of 11 children, so lack of access to a primary care provider created huge health setbacks for my family. My interests are internal medicine and studying patterns, treatments, and common clinical findings in infectious diseases. I am completing a residency in internal medicine, specifically hospital medicine in a rural hospital with a diverse population. I intend on practicing medicine within the chronic and acutely ill adult population at this hospital once I am done with my postgraduate training.